|
BLOG ARCHIVE
2020
2010-13
2009
2008
2007

|
BLOG:
June 2010 -
December 2013
I - Breast
cancer risk factors
3. Breast cancer
risk factors - overview
In the most simplified context, we can say that all it takes for
breast cancer - or any other - to start growing and keep growing unopposed
is two things:
(1) fatally compromised
cell-cycle integrity and
(2) immune system
insufficiency.
The former invariably involves malfunction of the cellular
DNA which, in turn, requires multiple
alterations to it, with the combined effect producing malignant cell. These
DNA alterations can be either passed through hereditary line (most
or, very seldom, all of them) or, much more often, result of a damage to
the DNA by carcinogens.
And such damage can only occur if all protective lines - set by
the body's detox system and body's
oxidative protection - fail. This can
protective inefficiency may and may not
be due to the great magnitude of exposure to the carcinogen.
Finally, the damage only counts if repair mechanism, for whatever
reason, fails.
So, the typical cancer path is:
multiple exposure to carcinogen ▶
multiple protective systems failure
▶
accumulated DNA damage/repair failure
▶
malignant cell cycle alteration ▶
immune system failure ▶
cancer
Considering how incredibly complex all this is - from the
protective systems to the cell cycle and immune system - it is
no wonder that the list of known or suspected breast cancer risk
factors is a mile long. In order to make it easier to grasp, these factors
can be grouped according
to their primary role in the disease.
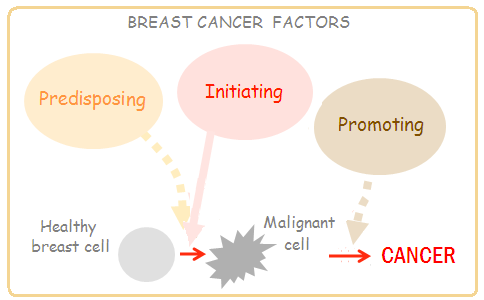
Those that exist before the cancer forms are
predisposing
breast cancer risk factors.
Those that actually push the cell into cancerous transformation
by damaging or inhibiting some of its vital functions, are
initiating
factors, or carcinogens.
And those that in some way stimulate or make easier growth and proliferation of
the existing cancerous cells are breast cancer
promoting factors.
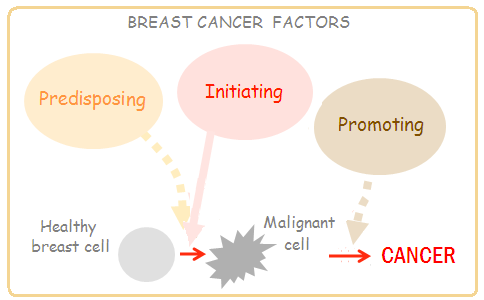
The distinction is often vague, since predisposing factors before
cancerous transformation often become promoting factors after it.
Most of the factors involved with breast cancer formation can have
such a dual role.
Following is a lists of major breast cancer risk factors grouped
according to this general scheme, with each factor given an expanded
window in a table below.
BREAST CANCER
RISK
FACTORS
(A) PREDISPOSING
1 -
Compromised detox system
(including body's oxidative protectioon)
due to toxic overload and nutritional deficiencies,
chronic
stress and/or negative
emotions
2 -
Compromised oxidative protection
3
- Genetic polymorphism compromising neutralization
of carcinogens, DNA
repair and cell cycle control
4 - Compromised immune system increasing
likelihood of an
active viral infection
5 - Other
Nutritional deficiencies/imbalances
Regular alcohol consumption
Smoking
(C)
PROMOTING
1 - Compromised immune function due to chronic
stress, negative
emotions
and/or
chronic
internal infections
2 -
Compromised detox system
due to toxic overload and nutritional deficiencies,
chronic
stress and/or negative
emotions
3 - Mitogenic/antiapoptopic hormones
Ovarian hormones high/unbalanced
Hormonal medical treatments
Exposure to environmental estrogens
Elevated insulin
Elevated IGF
4
- Genetic polymorphism compromising cell cycle
control
and immune
system efficiency
5 - Other
Nutritional deficiencies/imbalances
Regular alcohol consumption
Smoking
Low melatonin due to lack of sleep
Wearing bra extensively
Obesity/weight gain (postmenopausal)
Lean body (premenopausal)
Insufficient/inadequate checkups
|
(A) FACTORS
PREDISPOSING FOR BREAST
CANCER
|
|
A1 -
Compromised detox system |
|
toxic overload |
●
toxins from food,
air, water, dental implants, medications, internal
microorganisms. Overburdened and/or compromised by
genetic/nutritional deficiencies detox system can't
efficiently metabolize and dispose of toxins; toxic
metabolites inflict injury by causing oxidative damage or
cross-linking with body molecules, including DNA |
|
nutritional deficiencies |
●
detox function is dependant on the wide spectrum of
nutrients |
|
chronic
stress
psychological trauma |
●
negatively affects entire metabolism, detox and
other functions |
|
negative
emotions |
●
negative
self-image,
pessimism, suppression of emotions,
poor organizing |
|
chronic dehydration |
●
sufficient water intake is a must for efficient
detox function |
|
A2 - Compromised
oxidative protection |
|
oxidative exposure |
●
tobacco smoke, chlorine, pesticides, food additives,
drugs, air pollutants, heavy metals, ultraviolet
light... |
|
nutritional deficiencies |
●
oxidative protection depends on many
antioxidant nutrients |
|
A3 - Inherent genetic
aberrations |
|
BRCA1/2 gene mutation
|
●
tumor-suppressor genes, short for BReast
CAncer; mutation increases the risk up to
tenfold; estimated 5-10% of all breast cancer cases
carry mutated BRCA1 or 2
|
|
ATM gene
mutation
|
● also part
of tumor-suppressing mechanism, Ataxia-telangiectasia
mutated gene is estimated to be altered
(heterozygous carriers) in up to 1% of women; up to 10% of all breast
cancer cases are carriers, possibly more |
|
CHEK2 gene
mutation |
● cell
cycle checkpoint regulator gene, acting on
signals of DNA damage to prevent cellular division;
functionally associated with BRCA1 and TP53; its
1100delC heterozygous polymorphism has estimated <1% incidence
and threefold increase in breast cancer risk |
|
TP53 gene
mutation |
● tumor
(suppressor) protein p53 gene is mutated in
more than half of all cancers, but only in about 20% of
breast cancer cases; however, research indicates
that TP53 mutations are nearly three times more
frequent in BRCA1/2 germline mutation carriers;
TP53 is regulated by CHEK2 (which is, in turn,
activated by ATM), which activates TP53 to arrest
cell cycle for an attempt at DNA repair, and then
breaks it down to prevent apoptosis (programmed cell
death) if repair succeeds; illustrates genetic
interactions and interdependency
|
|
FOK1 gene
mutation |
● vitamin D
receptor gene, whose proper function is needed for
efficient cellular use of vitamin D, which inhibits
cell proliferation, and downregulates both
estrogen and progesterone receptors; significantly
lower risk increase than for above polymorphisms (indicated ~25% for Ff and ~60%
for ff FOK1 polymorphism), but much higher incidence
(about
40-50% and 10%, respectively) |
|
PALB2 gene
mutation |
● partner
and localizer of BRCA2 protein enables
accumulation of BRCA2 protein in the cell nucleus;
it is altered in less than 1% of women, doubling the
risk of breast cancer |
|
PTEN
gene mutation
|
● another
gene encoding tumor-suppressing protein (phosphatase
and tension homolog enzyme), PTEN mutations are very
rare, usually associated with Cowden syndrome;
carriers have up to 6 times higher breast cancer
lifetime risk
|
|
A4 - Compromised
immune system |
|
chronic
stress |
●
stimulates production of adrenal hormones,
inhibiting immune function, shrinking the thymus
gland and weakening antiviral response |
|
chronic
internal infections,
intestinal bacterial/fungal overgrowth,
insufficient rest (sleep)
time,
high sugar intake,
high blood lipids,
nutritional deficiencies, smoking, alcohol,
overweight,
negative
emotions |
●
poor lifestyle choices
negatively affect the immune function |
|
A4 - Other
predisposing factors |
|
nutritional deficiencies/imbalances |
●
compromising detox, antioxidative,
and/or cellular function |
|
regular alcohol consumption |
●
regular,
even quite moderate consumption inked with
higher blood estrogen levels; other possible
mechanisms include increased solubility of
carcinogens, interfering with folate metabolism,
elevated oxidative stress and mutagenic effects of
its primary metabolite, acetaldehyde |
|
tobacco smoke |
●
contains over 4000 chemicals, most of them toxic,
and over 50 known carcinogens |
(B) FACTORS INITIATING BREAST CANCER
(CARCINOGENS)
|
|
B1 - Radiation exposure |
|
early-life
medical exposures |
● radiation
exposures before age 20, beginning with fetal
exposures and subsequent X-ray and nuclear medicine
diagnostic (γ-rays)
exposures |
|
mammography |
● cumulative
doses in extended periods of time can be significant |
|
galactography |
● imaging of
breast's milk ducts by mammography unit; similar
exposure as low-level mammography |
|
other adult chest
or whole body exposures |
● other
radiology diagnostic procedures, occupational
exposures, nuclear fallout, smoking (from Polonium
210), air travel, radon, background radiation
|
|
non-ionizing radiation
(power field) |
● although
the evidence is inconclusive, there are clear
indications that exposure to non-ionizing radiation can
be significant breast cancer risk factor |
|
|
|
sexual intercourse,
physical contact, food (grains),
pets (?) |
● human
papilloma virus (HPV), mouse mammary tumor virus (MMTV),
Epstein-Barr virus (EBV) and bovine leukemia virus (BLV)
have been identified at higher to much higher
incidence in breast cancer patients; each has the
ability to alter cellular DNA, transforming normal
cells into malignant |
B3 - Chemical carcinogens
|
|
industrial chemicals (including food additives,
pesticides and herbicides) in construction and
household products, food, water and environment |
● many chemicals have been
identified as carcinogenic, mainly in experiments
with laboratory animals; little research is done on
the role of unknown number of such chemical
carcinogens in the initiation and growth of breast
cancer, but it is reasonable to assume it to be
significant |
(C) FACTORS PROMOTING BREAST
CANCER
|
|
C1
- Mitogenic/antiapoptopic
hormones |
|
ovarian hormones
level/balance |
● nominal
blood estrogen level is an indicator, although
somewhat loose, of the free (bioavailable, active)
estrogen, which stimulates cell proliferation;
higher estrogen level is likely to result in early
menarche and late menopause (also, as a part of the
elevated overall hormonal activity, in accelerated
growth)
● hormonal balance is regulated
by a complex co-action of the pituitary gland and
hypothalamus, but also affected by other factors,
such as exposures to xenoestrogens (environmental
estrogens) or chronic stress |
|
exposure to
environmental estrogens (xenoestrogens) |
●
Phthalates
(plasticizers)
-
chemicals
leaking into foods form plastic containers and
wraps, tend to accumulate in the body and may
disrupt endocrine function
●
Pesticides
- present in
many foods and drinking water, may negatively affect
body's regulatory functions, including hormonal
●
Detergents,
trichloro-ethylene,
PCBs...
many
environmental chemicals can act as estrogen mimics;
level of exposure and individual vulnerability vary,
but can be significant
●
Cadmium
- toxic contaminant present in
food, water and environment (also, in tobacco) that
steadily accumulates in the body, acting like
estrogen; it can also raise testosterone levels, as
additional breast cancer risk factor
●
Natural food components - some natural food components,
for instance, soybean isoflavones genistein and
daidzein, can have estrogenic effect; however, Asian populations
with high soybean intake have low breast cancer
incidence, which suggests that (1) the effect may be
more complex, and/or dependant on the overall diet
and lifestyle (2) soy isofavones generally act as
anti-estrogens, taking estrogen receptors while
having much lower estrogenic potency (less than 2%)
●
Herbal extracts - natural
herbal components can also have estrogenic potency;
among commonly used herbs with such compounds are
angelica, reishi mushroom, licorice, fo-ti and
astragalus (they are all considered healthful, hence
the above applies here as well) |
|
elevated insulin |
From
high-glycemic diet,
insulin resistance, diabetes;
insulin
stimulates cell division and increases the level of
free (active) estrogen |
|
elevated IGF |
insulin-like growth
factor, mitogenic,
antiapoptotic hormone, enhancing estrogen activity,
and vice versa; high
levels linked to increased risk of several common
cancers, including breast cancer |
|
hormonal medical
treatments |
●
lHRT
-
large trials consistently come up with significantly
increased risk
●
Birth
control
pills - the earlier
in life starts the use, and the longer it lasts, the
more of the risk factor they become
●
SERM drugs -
Selective
Estrogen Receptor Modulator,
including those like Tamoxifen, that are used for
breast cancer treatment and prevention, evidently
are the additional risk factor for some
woman |
|
C2 -
Compromised immune function |
|
chronic
internal infections |
●
toot/jaw/root canal infections
-
appears to
have significantly higher incidence in breast cancer
patients |
|
intestinal bacterial/fungal overgrowth |
● often
accompanied with
leaky gut
and nutritional deficiencies, burdens and
weakens the immune system |
|
chronic
stress |
●
stimulates production of adrenal hormones,
inhibiting immune function, shrinking the thymus
gland and weakening protective responses against
cancer |
|
insufficient rest (sleep) time,
high sugar intake,
high blood lipids, nutritional deficiencies,
smoking, alcohol, overweight, negative
emotions |
●
many poor lifestyle choices alone negatively affect
immune function, and their combined negative effect
is disproportionally larger |
|
C3 -
Compromised detox system |
|
●
due to toxic overload, toxic intestines
(bacterial/fungal overgrowth), leaky gut, nutritional deficiencies,
chronic
stress and/or
negative
emotions,
chronic dehydration
|
|
C4 -
Genetic
aberrations |
|
●
compromising cell cycle control
and immune
system efficiency |
|
C5 -
Other promoting factors |
|
nutritional deficiencies/imbalances |
●
high-glycemic diet
- causing
elevated blood level of both, insulin (with or
without insulin insensitivity) and IGF, which promotes cell
proliferation similarly to estrogen
●
high-sugar
diet - in addition to
being a high-glycemic food, sugar inhibits the
immune system; higher rate of glycolysis (burning
glucose for energy within cell) increases
concentration of its by-product, lactic acid, making
cell more acidic, hence compromising its optimum
functioning
●
low fiber - evidence
supports inverse relationship between
dietary fiber
intake and breast cancer risk
●
specific mineral/vitamin
deficiencies compromising detox, immune,
and/or cellular function
|
|
regular alcohol consumption |
●
regular,
even quite moderate consumption inked with
higher blood estrogen levels; other possible
mechanisms include increased solubility of
carcinogens, interfering with folate metabolism,
elevated oxidative stress and mutagenic effects of
its primary metabolite, acetaldehyde |
|
smoking |
●
contains over 4000 chemicals, most of them toxic,
and over 50 known carcinogens |
|
low melatonin |
● melatonin
is an estrogen antagonist hormone; it also acts as
antioxidant, antimitotic and immune-enhancing agent;
body produces melatonin mainly during nighttime
sleep, in darkness; thus lack of nighttime sleep, or
lighted room, inhibit melatonin production, and so
does exposure to power (electrical) field |
|
breast
compression |
● the risk
seems to become the more significant the longer bra
is worn over several hours a day, on daily basis |
|
overweight/obesity |
● according
to research data, overweight and obesity are risk
factors for postmenopausal women; |
|
weight gain (postmenopausal) |
●
can enhance estrogen production and lead to estrogen
dominance state |
|
lean body (premenopausal) |
●
if resulting from
diet
restriction,
metabolic disturbance or deficiency |
|
insufficient/inadequate checkups |
● latter
stages at the time of diagnosis significantly lower chances
for recovery
● risk of
false negatives,
compression risk,
radiation risk |
The above list of breast cancer risk factors, as
overwhelming as it is, is neither complete nor clear
with respect to mechanisms leading to carcinogenic
transformations. It is barely scratching the surface of the
complexity behind the onset and progress of this disease. Many factors are involved, and
their
significance and interplay can vary greatly
from one individual
to another.
In addition, there are certainly some pieces of the
puzzle that we are still unaware of. But what is known so far is
both, best reference and best starting point for understanding the
disease, and for taking steps to efficiently minimize the risk
of becoming a part of the breast cancer statistic.
Obviously, there is much more that can be said about each of
these factors. That journey starts with the
following
page.
TOP
NEXT
YOUR BODY
┆ HEALTH
RECIPE
┆ NUTRITION ┆
TOXINS ┆
SYMPTOMS
|